– What is the significance of drug resistance among newly diagnosed HIV-1 patients in Luanda?
Title: Uncovering the Diversity of HIV-1 and Drug Resistance in Newly Diagnosed Patients in Luanda, Angola: The Impact of Integrase Inhibitors
In recent years, there has been a growing concern about the prevalence of HIV-1 and drug resistance in newly diagnosed patients in Luanda, Angola. With the increasing number of reported cases, it has become crucial to explore the diversity of HIV-1 strains and the effectiveness of different antiretroviral treatments in this region. One area of interest is the impact of integrase inhibitors, a class of antiretroviral drugs that target the integrase enzyme of HIV-1, on the management of the disease.
The Diversity of HIV-1 Strains in Luanda, Angola
Luanda, the capital city of Angola, is a vibrant and diverse urban center with a population that exceeds 8 million people. The city has a high prevalence of HIV-1, with a significant number of newly diagnosed cases reported each year. One of the key challenges in managing HIV-1 in Luanda is the genetic diversity of the virus, which can impact the efficacy of antiretroviral therapy (ART) and increase the risk of drug resistance.
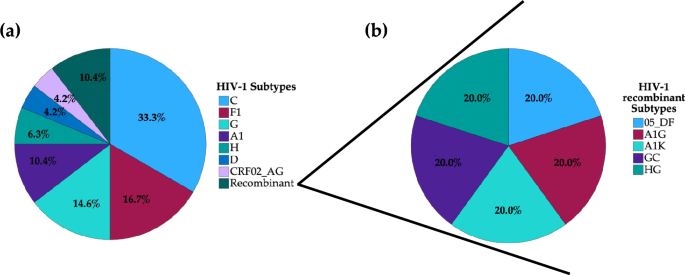
HIV-1 strains are classified into different subtypes and circulating recombinant forms (CRFs), with subtype C being the most common in Southern Africa, including Angola. However, recent studies have shown a significant diversity of HIV-1 strains in Luanda, with multiple subtypes and CRFs circulating among newly diagnosed patients. This diversity can have implications for treatment outcomes, as different strains may respond differently to antiretroviral drugs.
The Impact of Drug Resistance on HIV-1 Treatment
Drug resistance is a major concern in the management of HIV-1, as it can limit the effectiveness of antiretroviral drugs and lead to treatment failure. In Luanda, the prevalence of drug resistance among newly diagnosed patients is a growing issue, with resistance mutations detected in a significant proportion of individuals starting ART. This highlights the importance of regular monitoring of drug resistance in HIV-1 patients to guide treatment decisions and prevent the spread of resistant strains.
Integrase inhibitors are a newer class of antiretroviral drugs that have shown promising results in the treatment of HIV-1. These drugs work by blocking the integrase enzyme, preventing the virus from inserting its genetic material into the host cell’s DNA. Integrase inhibitors have been shown to be effective in reducing viral load and increasing CD4 cell count in patients with HIV-1, making them an important component of modern ART regimens.
The Role of Integrase Inhibitors in Managing HIV-1 in Luanda
In the context of the diversity of HIV-1 strains and drug resistance in Luanda, integrase inhibitors offer a valuable treatment option for newly diagnosed patients. These drugs have been shown to be effective against a wide range of HIV-1 strains, including those with resistance mutations to other classes of antiretroviral drugs. Integrating integrase inhibitors into ART regimens can help improve treatment outcomes and reduce the risk of virological failure in patients with diverse HIV-1 strains.
Studies have also shown that integrase inhibitors have a favorable safety profile and are generally well-tolerated by patients. This makes them a suitable choice for long-term treatment of HIV-1 in resource-limited settings like Luanda, where adherence to ART regimens can be a challenge. By incorporating integrase inhibitors into HIV-1 treatment protocols, healthcare providers in Luanda can enhance the quality of care for newly diagnosed patients and improve overall treatment outcomes.
Conclusion
the diversity of HIV-1 strains and drug resistance in newly diagnosed patients in Luanda, Angola, presents a significant challenge for healthcare providers and researchers. By understanding the impact of integrase inhibitors on the management of HIV-1 in this region, we can improve treatment outcomes and mitigate the spread of drug-resistant strains. Integrating integrase inhibitors into ART regimens can help address the genetic diversity of HIV-1 and enhance the effectiveness of treatment for patients in Luanda.
Recent Research on HIV Drug Resistance and Transmission Dynamics
With the continuous evolution of HIV-1 within hosts, the impact on transmission dynamics has become a critical area of study. Researchers like K. Theys et al. have delved into this subject in-depth, highlighting the intricate relationship between viral evolution and transmission patterns (“Theys, K. et al., 2018”).
In Africa, HIV drug resistance has emerged as a pressing concern that demands urgent attention, as outlined by Moreno et al. in their work on this topic (“Moreno, M. et al., 2017”). WHO’s “HIV Drug Resistance Report 2021” further emphasizes the global significance of this issue (WHO, 2021).
Analyzing the molecular epidemiology of HIV-1 from 1990 to 2015, Hemelaar et al. conducted a comprehensive review that sheds light on global and regional trends in infection patterns (“Hemelaar, J. et al., 2018”). These findings provide valuable insights for public health strategies and intervention programs.
UNAIDS Data from 2023 paints a current picture of the HIV landscape, offering crucial data for policymakers and healthcare providers to address the ongoing challenges (“UNAIDS, 2023”). Additionally, studies like that by Sebastião et al. on genetic diversity and drug resistance among pregnant women in Angola provide localized insights into the issue (“Sebastião, C. S. et al., 2019”).
To combat the rise of HIV drug resistance in low and middle-income countries, researchers stress the importance of dolutegravir-containing regimens like those discussed in the Lancet Infectious Diseases publication by Inzaule et al. (“Inzaule, S. C. et al., 2019”). Detecting low-abundance drug-resistant HIV-1 variants in individuals who are treatment-naive is a crucial step in managing resistance development, as highlighted in a systematic review by Mbunkah et al. (“Mbunkah, H. A. et al., 2020”).
Technological advancements in sequencing, such as population-based nanopore sequencing of the HIV-1 pangenome, have offered new avenues for identifying drug resistance mutations, thereby enhancing our understanding and management of resistance (“Ode, H. et al., 2024”). Wang et al.’s work on nanopore sequencing technology further underscores the transformative potential of this approach (“Wang, Y. et al., 2021”).
In the realm of genotypic-resistance testing interpretation, resources like those compiled by Liu and Shafer have proven invaluable for clinicians and researchers in making informed treatment decisions (“Liu, T. F. & Shafer, R. W., 2006”). Additionally, de Soldi et al.’s study on major drug resistance mutations to HIV-1 protease inhibitors highlights the challenges in managing resistance in real-world clinical settings (“de Soldi, G. F. R. et al., 2019”).
With the development of multiplex PCR methods for sequencing virus genomes directly from clinical samples, as demonstrated by Quick et al., the field of genomics has been revolutionized, enabling rapid and accurate characterization of viral strains (“Quick, J. et al., 2017”). Johnson’s work on an extended IUPAC nomenclature code for polymorphic nucleic acids further enhances our ability to accurately describe and analyze genetic variations (“Johnson, A. D., 2023”).
the landscape of HIV drug resistance and transmission dynamics is constantly evolving, and ongoing research efforts are essential to address these challenges effectively. By leveraging cutting-edge technologies and collaborative strategies, we can make significant strides in combating HIV and enhancing global public health outcomes.Research on HIV Drug Resistance Genotyping
In recent years, there has been significant progress in automating HIV drug resistance genotyping to enhance clinical management and surveillance of HIV-1 infections. Various research studies have explored the use of advanced sequencing technologies to track drug resistance mutations and inform treatment decisions effectively.
Automated Tools for Genotyping
One study by Woods et al. (2012) introduced RECall, a freely accessible sequence analysis tool for automating HIV drug resistance genotyping. This tool revolutionized the process by providing a more efficient and accurate method for identifying drug resistance mutations.
Next-generation sequencing has also been applied to track HIV-1 drug resistance mutations in specific regions, such as Portugal, as demonstrated by Pimentel et al. (2024). This approach allows for the rapid identification of circulating drug resistance mutations, enabling timely interventions.
Performance Evaluation of Genotyping Tools
Pineda-Peña et al. (2013) evaluated the performance of various automated subtyping tools, including the new REGA version 3, for clinical and surveillance purposes. Their findings highlighted the importance of accurate and reliable genotyping tools in managing HIV drug resistance effectively.
In another study, Struck et al. (2014) proposed COMET, an adaptive context-based modeling approach for ultrafast HIV-1 subtype identification. This method aims to streamline the process of identifying subtype-specific drug resistance mutations for targeted interventions.
Monitoring Transmitted Drug Resistance
Tzou et al. (2020) focused on monitoring transmitted HIV-1 drug resistance mutations, particularly in the context of integrase strand transfer inhibitors (INSTIs). Their research underscores the importance of surveillance in identifying emerging drug resistance patterns and guiding treatment decisions.
Advancements in Alignment and Annotation
Libin et al. (2019) introduced VIRULIGN, a fast codon-correct alignment tool for viral genomes. This tool enables researchers to align and annotate viral sequences accurately, facilitating the identification of drug resistance mutations and genetic variations.
FastTree by Price et al. (2009) offers a novel approach to computing large minimum evolution trees using profiles instead of a distance matrix. This method enhances the speed and efficiency of phylogenetic analysis, aiding in the identification of evolutionary relationships among viral strains.
Current Trends in Drug Resistance Research
Recent studies have focused on primary resistance to integrase strand transfer inhibitors in diverse HIV-1 subtypes, particularly in sub-Saharan Africa (Inzaule et al., 2018). This research sheds light on the challenges and implications of drug resistance in different geographical regions.
A Comprehensive Review of Drug Resistance
Mbhele et al. (2021) provided a comprehensive review of HIV-1 integrase strand transfer inhibitors, highlighting current treatment options, recent advances, and emerging drug resistance trends. This review serves as a valuable resource for clinicians and researchers in managing drug-resistant HIV infections.
Future Perspectives and Recommendations
With the increasing prevalence of drug resistance mutations, continuous monitoring and surveillance are essential to guide effective treatment strategies. Studies like those by Ntamatungiro et al. (2022) and Arimide et al. (2022) emphasize the importance of pre-treatment resistance testing and understanding natural polymorphisms to optimize treatment outcomes.
advancements in automated genotyping tools, sequencing technologies, and alignment methods have revolutionized the field of HIV drug resistance research. By leveraging these innovative tools and approaches, researchers can gain insights into drug resistance mechanisms and tailor treatment regimens to individual patient needs.
The Impact of HIV-1 Drug Resistance: A Comprehensive Analysis of Recent Studies
In recent years, the issue of HIV-1 drug resistance has become a major concern, as highlighted by various studies conducted in different regions around the world. These studies shed light on the genetic diversity of HIV-1 strains and the mutations that confer resistance to antiretroviral drugs.
Recent Research Findings
One study conducted in Nigeria by Oluniyi, P. E. et al. (2022) examined HIV-1 drug resistance and genetic diversity in a cohort of people living with HIV-1. The study revealed the presence of drug resistance mutations in the population, emphasizing the need for effective treatment strategies.
Similarly, Mikasi, S. G. et al. (2021) analyzed drug resistance mutations in HIV-1 integrase sequences from Cameroon. The findings of this study underscored the importance of monitoring drug resistance trends to inform clinical practice and public health interventions.
In South Africa, Obasa, A. E. et al. (2020) investigated drug resistance mutations against protease, reverse transcriptase, and integrase inhibitors in individuals receiving boosted protease inhibitors. The study provided valuable insights into the prevalence of drug resistance in this population.
Transmitted Drug Resistance
Studies conducted in other regions, such as Porto Alegre, South Brazil, by Nunes, C. C. et al. (2022) have also examined transmitted drug resistance to integrase strand transfer inhibitors in newly diagnosed adults. These findings contribute to our understanding of the dynamics of drug resistance transmission.
Baseline HIV Drug-Resistance Testing
In the United States, Hugueley et al. (2022) conducted a study on baseline HIV drug-resistance testing in 12 jurisdictions. The study highlighted the importance of routine resistance testing to guide treatment decisions and improve patient outcomes.
Future Directions in Research
Looking ahead, it is crucial to continue monitoring HIV-1 genetic diversity and drug resistance mutations, as highlighted in studies from Angola by Sebastião, C. S. et al. (2021) and Afonso, J. M. et al. (2012). These studies emphasize the need for ongoing research to address the evolving challenges of drug resistance in different populations.
the diverse range of studies on HIV-1 drug resistance provides valuable insights into the current landscape of resistance mutations and genetic diversity. By staying informed about the latest research findings, healthcare providers and policymakers can develop effective strategies to combat drug resistance and improve treatment outcomes for individuals living with HIV-1.
HIV drug resistance: Insights from Recent Studies
Recent studies have shed light on the issue of HIV drug resistance, providing valuable insights into this ongoing global health challenge. The following research findings contribute to our understanding of HIV drug resistance and its implications for treatment and prevention strategies.
Surveying Transmitted HIV-1 Drug Resistance
In a 2009 update, Bennett et al. conducted a study on drug resistance mutations to monitor transmitted HIV-1 drug resistance. This research aimed to enhance surveillance and tracking of drug-resistant strains of the virus, helping to inform treatment protocols and minimize the spread of resistant strains.
Understanding HIV-1 Protease Mutations and Cross-Resistance
Rhee et al. investigated HIV-1 protease mutations and their impact on protease inhibitor cross-resistance in a 2010 study. This research delved into the molecular mechanisms underlying drug resistance and the potential for cross-resistance among various antiretroviral medications.
Predicting Co-Receptor Tropism in HIV-1 Subtype C
A more recent meta-analysis by Matume et al. in 2020 focused on predicting co-receptor tropism in HIV-1 subtype C in Africa. By analyzing individual sequence data, this study aimed to improve our understanding of viral tropism and its implications for treatment outcomes in different populations.
Exploring Factors Influencing HIV Drug Resistance in Pregnant Women
Sebastião et al. conducted a cross-sectional study in 2021 to investigate the factors influencing HIV drug resistance among pregnant women in Luanda, Angola. Their findings highlight the importance of addressing specific risk factors and implementing targeted interventions to prevent drug resistance in this vulnerable population.
Examining the Impact of HIV-1 Infection in Sub-Saharan Africa
Buvé et al. explored the spread and effect of HIV-1 infection in sub-Saharan Africa in a landmark study published in 2002. Their findings underscore the significant burden of HIV in this region and emphasize the need for comprehensive prevention and treatment strategies to curb the epidemic.
Conclusion
These studies provide valuable insights into the complex landscape of HIV drug resistance and highlight the ongoing challenges in managing and preventing resistance development. By continuing to research and monitor drug resistance patterns, we can better tailor treatment approaches and public health initiatives to address this critical issue.