Introduction
As the global fight against tuberculosis (TB) continues to evolve, the emergence of drug-resistant strains presents a formidable challenge for public health systems worldwide. In Ningbo, China—a rapidly industrializing city with a population exceeding 8 million—researchers are turning their attention to understanding the transmission dynamics of drug-resistant tuberculosis through a combination of epidemiological tracking adn genomic analysis. this complete study, featured in the journal Frontiers, delves into the complex interactions between human behavior, healthcare access, and the genetic mutations that enable TB to evade standard treatments. By shedding light on the patterns of resistance and transmission, this research aims to inform more effective interventions and policy decisions, ultimately contributing to global efforts to curb this persistent public health threat. In an era where antimicrobial resistance is rising to unprecedented levels, uncovering the nuances of TB in urban settings like Ningbo is crucial for crafting targeted strategies to combat the disease. This article explores the findings of the study, the methodologies employed, and the implications for the future of TB management both locally and globally.
Understanding the Epidemiological Landscape of Drug-Resistant Tuberculosis in Ningbo
The epidemiological landscape of drug-resistant tuberculosis (DR-TB) in Ningbo reveals a complex interplay between transmission dynamics and the socio-environmental factors that influence the spread of this resilient pathogen. Recent studies highlight a concerning increase in the prevalence of DR-TB, driven by a variety of factors including inadequate healthcare access, mismanagement of treatment protocols, and socioeconomic disparities. Understanding these contributors is critical for formulating effective public health interventions.
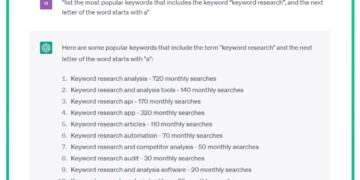
Furthermore, genomic analysis has proven essential in delineating the transmission pathways of DR-TB strains within the region. By utilizing whole-genome sequencing, researchers can track mutations responsible for drug resistance and identify clusters of transmission among populations. This rich data can inform targeted strategies such as the implementation of enhanced surveillance measures and practical treatment guidelines, ultimately aiming to curb the rising tide of drug-resistant strains in the community.
| Factors Influencing DR-TB | Description |
|---|---|
| Healthcare Access | Variability in access to quality TB care can exacerbate DR-TB spread. |
| Treatment protocols | Inconsistent adherence to treatment regimens leads to resistance advancement. |
| Socioeconomic Status | Poverty and lack of education are linked to higher infection rates. |
| Genomic Surveillance | Enable tracking of transmission and resistance patterns. |

Genomic Insights into the Mechanisms of resistance in Mycobacterium tuberculosis
Recent genomic analyses have revealed intricate mechanisms that facilitate resistance in Mycobacterium tuberculosis (MTB),notably in the context of emerging drug-resistant strains. By sequencing the genomes of resistant and susceptible isolates from the Ningbo region, researchers have been able to identify specific mutations associated with resistance to key antitubercular drugs like isoniazid and rifampicin. These mutations often occur in genes such as katG and rpoB,and their presence can significantly diminish the efficacy of treatment options. Understanding these genomic variations is crucial for tailoring appropriate therapeutic strategies and for anticipating the evolution of resistance profiles in local populations.
The study also highlights the importance of horizontal gene transfer and intragenic evolution, which contribute to the dynamic landscape of drug resistance in MTB. Identifying factors that lead to transmission of resistant strains within communities is essential. Crucial findings include:
- Clonal Lineages: Distinct clonal lineages associated with resistance were identified, suggesting localized transmission patterns.
- Co-infection Rates: Elevated co-infection rates with HIV complicate treatment protocols, necessitating integrated approaches.
- Mutational Hotspots: Specific regions within the genomes were found to be mutation hotspots,indicating areas where monitoring efforts should be intensified.
This genomic insight not only enriches our understanding of MTB resistance mechanisms but also underscores the importance of ongoing surveillance and genomic monitoring to mitigate the impacts of drug-resistant tuberculosis.

Transmission Pathways and Risk Factors Contributing to Drug-Resistant Strains
Understanding the dynamics of drug-resistant tuberculosis (TB) transmission involves examining various pathways and risk factors that facilitate the spread of resistant strains within communities. In Ningbo, China, several key factors influence the proliferation of drug-resistant TB, including inadequate treatment adherence, high population density, and socioeconomic disparities. These elements create an habitat conducive to the survival and transmission of resistant bacterial strains, exacerbating the public health challenge. Furthermore, the role of healthcare infrastructure cannot be overlooked, as gaps in diagnostic capabilities and access to effective treatment options further contribute to the transmission of drug-resistant cases.
Among the various pathways, person-to-person transmission remains the most notable mode of spreading drug-resistant TB, particularly in high-risk groups such as immunocompromised individuals and those with a history of previous infections. The interplay of genetic factors in certain populations also enhances susceptibility to acquiring drug-resistant TB strains. Below is a summary of notable risk factors identified in the epidemiological analysis conducted in Ningbo:
| Risk Factor | Description |
|---|---|
| inadequate Treatment | Failure to complete treatment courses leading to resistant strains. |
| Healthcare Gaps | Lack of access to quality TB care and diagnostics. |
| Social Determinants | Poverty and living conditions that increase exposure. |
| Comorbid Conditions | medications or conditions that compromise the immune system. |

Implications for Public Health Strategies in Controlling Tuberculosis in Ningbo
Considering the findings regarding drug-resistant tuberculosis (DR-TB) transmission dynamics in Ningbo, public health strategies must be reformed to effectively combat this escalating health crisis. The epidemiological data reveals a significant correlation between genomic mutations and the persistence of DR-TB strains, emphasizing the necessity for targeted interventions. Key strategies should include:
- Enhanced Surveillance: Implement comprehensive monitoring systems to track TB cases, especially those resistant to first-line treatments.
- Strengthened Diagnostics: Invest in rapid molecular diagnostics that can identify drug resistance at the onset of infection.
- Community Engagement: Increase awareness campaigns to educate the public about TB symptoms, importance of compliance with treatment, and routine screening practices.
- Collaboration with Healthcare Facilities: Ensure that hospitals and clinics are equipped with adequate personnel and resources to manage and treat DR-TB cases effectively.
Additionally, integrating genomic analysis into routine public health measures can provide invaluable insights into the transmission pathways of DR-TB. For instance, by mapping the spread of strains through genomic sequencing, health officials can identify hotspots for intervention. This can be further supported by establishing a multi-disciplinary task force aimed at improving treatment protocols, as outlined below:
| Focus Area | Action Steps |
|---|---|
| Patient Care | Revise treatment guidelines to include newer drug regimens for resistant cases. |
| Research Funding | Allocate resources towards studies exploring the genetic profiles of local strains. |
| Policy Development | Formulate policies that promote access to medicines and equitable TB care. |

recommendations for Future research and Surveillance initiatives
The ongoing challenges posed by drug-resistant tuberculosis (TB) in Ningbo,China,highlight the urgent need for comprehensive future research and surveillance initiatives. Enhanced frameworks could significantly improve our understanding of transmission dynamics, which would be crucial in informing public health strategies. Future studies should focus on:
- Longitudinal studies to monitor trends in drug resistance over time and understand the implications for treatment regimens.
- Socioeconomic factors influencing TB transmission, which could aid in identifying high-risk populations.
- Integration of genomic surveillance with epidemiological data to pinpoint specific mutations conferring drug resistance.
- Cross-regional comparisons within China to assess differences in TB transmission dynamics and resistance patterns.
In addition to research, improving surveillance initiatives is essential for controlling TB. Implementing a centralized data-sharing system among healthcare institutions can enhance the tracking of TB cases. Proposed enhancements include:
- Real-time data collection on drug resistance profiles to facilitate rapid response measures.
- Increased collaboration between local and national health authorities to ensure consistent monitoring and reporting protocols.
- community engagement programs aimed at raising awareness about TB prevention and treatment options.
- Development of a mobile request for frontline workers to report cases and access the latest guidance on managing drug-resistant TB.
Strengthening Healthcare Responses to Combat Drug-Resistant Tuberculosis Challenges
In the ongoing battle against drug-resistant tuberculosis (DR-TB), understanding the transmission dynamics within specific regions is crucial for tailoring effective public health interventions.The study conducted in Ningbo, China, provides vital insights into how DR-TB spreads within communities. Key findings highlight the importance of genomic surveillance, which reveals unique patterns of resistance and transmission that can inform targeted strategies.By leveraging data on transmission chains and infection hotspots, public health officials can enhance contact tracing efforts and allocate resources where they are needed most.
In addition to genomic data, the research underscores the significance of a multi-faceted approach to combat the challenges posed by DR-TB. Efforts should encompass the following strategies:
- Enhanced Screening and Diagnosis: Implementing rapid diagnostic tools to identify TB strains quickly.
- Patient Education: Raising awareness about drug resistance and promoting adherence to prescribed treatment regimens.
- Strengthened Healthcare Infrastructure: Investing in healthcare facilities to provide comprehensive TB management services.
- Collaboration with Global Health Initiatives: Engaging in partnerships that facilitate knowledge sharing and resource allocation.
these combined efforts can lead to a more robust healthcare response capable of mitigating the impact of drug-resistant forms of tuberculosis in affected regions.
In Summary
the comprehensive study of drug-resistant tuberculosis (TB) transmission dynamics in Ningbo, China, sheds new light on the complex interplay between genetics and epidemiology in managing this public health crisis. Through meticulous genomic analysis and an in-depth epidemiological approach, this research highlights both the challenges faced in controlling the spread of resistant TB and potential strategies for intervention.The findings underscore the urgent need for enhanced surveillance, tailored treatment protocols, and public health policies that address the unique characteristics of drug-resistant strains. As various cities grapple with the growing burden of TB, insights from Ningbo serve as a critical reminder of the importance of robust data-driven approaches to curb this persistent threat to global health. future research in this field is essential, paving the way for innovative solutions and ultimately steering us towards a world where tuberculosis can be effectively contained, irrespective of drug resistance.













Why Tokyo Misses the Iconic ‘Blade Runner’ Atmosphere Where It Counts Most