Rising Antibiotic Resistance in Helicobacter pylori: Emerging Challenges in Nanjing, China
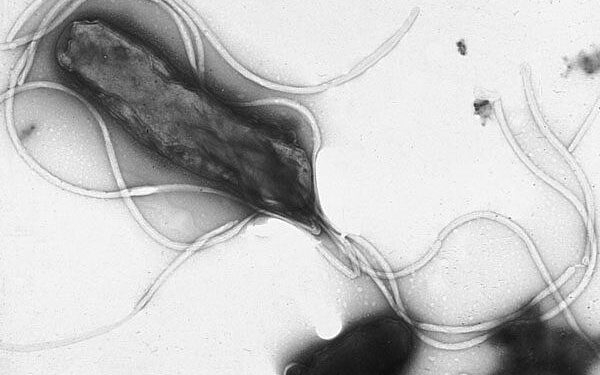
The global healthcare community is increasingly confronted with the daunting issue of antibiotic resistance, a phenomenon that complicates the management of infectious diseases. A recent comprehensive investigation conducted between 2018 and 2021 has brought to light critical insights into the escalating resistance of Helicobacter pylori—a bacterium implicated in numerous gastric ailments—within Nanjing, China. This study reveals troubling shifts in how H. pylori responds to commonly used antibiotics, signaling an urgent need for revised treatment protocols and enhanced public health strategies. Herein, we explore these findings and their implications for managing one of the most widespread bacterial infections worldwide.
Evolving Patterns of Antibiotic Resistance in Helicobacter pylori: Treatment Challenges in Nanjing
Over recent years, research has documented a marked increase in antibiotic resistance among H. pylori strains isolated from patients across Nanjing. Notably, resistance rates against frontline antibiotics such as clarithromycin, amoxicillin, and metronidazole have surged significantly by 2021—raising concerns about diminishing effectiveness of standard eradication therapies. These trends mirror global patterns where misuse and overuse of antibiotics—including self-medication and inappropriate prescriptions—have accelerated resistant strain emergence.
Understanding localized resistance profiles is vital for tailoring effective therapeutic regimens that reflect regional microbial dynamics rather than relying solely on generalized guidelines. Incorporating susceptibility testing into routine clinical practice can help clinicians select optimal treatments while minimizing unnecessary antibiotic exposure.
| Antibiotic | Resistance Rate (%) | Year Recorded |
|---|---|---|
| Clarithromycin | 29% | 2021 |
| Amoxicillin | 12% | 2021 |
| Metronidazole | 40% | 2021 |
Moreover, alternative treatment options such as bismuth-containing quadruple therapy are gaining traction due to their higher success rates amid rising drug resistance. Establishing ongoing surveillance systems will be crucial to track these evolving patterns continuously and inform evidence-based policy decisions.
How Patient Demographics Influence Antibiotic Resistance Trends in H. pylori Infections
The study further examined how demographic variables impact antibiotic resistance among infected individuals within Nanjing’s diverse population over three years:
- Younger Age Groups: Patients under 18 exhibited comparatively lower levels of resistant H. pylori strains—potentially reflecting less cumulative antibiotic exposure or differing infection sources.
- Males vs Females: Male patients were more frequently found harboring multidrug-resistant bacteria compared to females; this disparity may relate to behavioral or biological factors influencing infection risk or treatment adherence.
- Socioeconomic Status:Poverty-stricken communities showed higher prevalence rates for resistant infections possibly due to limited access to healthcare resources or incomplete treatments.
Geographical disparities within urban versus rural districts also emerged prominently; rural residents faced distinct challenges with elevated resistance frequencies complicating successful eradication efforts.
| Age Group (Years) | Resistance Rate (%) |
|---|---|
| 15% | |
| 23% | |
| 30% | |
| 45% |
These demographic correlations emphasize the necessity for personalized medical approaches that consider patient-specific factors when designing treatment plans aimed at overcoming antimicrobial hurdles posed by H.pylori infections.
Strategies To Mitigate Antibiotic Resistance And Improve Clinical Outcomes In Nanjing’s Healthcare Settings
Addressing this growing threat demands a coordinated response integrating multiple facets:
- Sustained Surveillance Programs:A continuous data collection framework tracking local antimicrobial susceptibility trends will enable timely updates on effective therapies.
- Epidemiological Education & Stewardship Training:Cultivating awareness among healthcare workers regarding prudent antibiotic use reduces unnecessary prescriptions fueling resistance development.
- Tightened Infection Control Protocols:The enforcement of stringent hygiene practices—including handwashing compliance, sterilization standards for medical instruments,and safe disposal methods—is essential within clinical environments.
- < strongCommunity Outreach Initiatives:
In parallel with these measures,the integrationof advanced diagnostic tools capableof rapidly identifying resistantH.pyloristrainswill empower clinicians tomake informed decisionsabout individualized therapy regimens.This precision medicine approach not only enhances cure rates but also helps preserve existing antibiotics’ efficacy by avoiding empirical broad-spectrum usage.Collaborative partnerships involving microbiologists,infection control specialists,and policymakersare indispensablefor mounting an effective defense against this public health menace.
Year Overall Resistance Rate (%) Predominant Resistant Antibiotics 2018 22% Clarithromycin , Amoxicillin 2019 25% Levofloxacin , Metronidazole 2020 30% Tetracycline , Nitroimidazoles 2021
< tdstyle =" text -align : center ; ">35 %
< tdstyle =" text -align : center ; ">Clarithromycin , LevofloxacinFinal Thoughts: Confronting The Growing Threat Of Antimicrobial Resistance In Helicobacter pylori Infections
In summary,the surge in drug-resistant Helicobacter pyloristrains identified through this extensive analysis fromNanjingsignifiesa pressing challengefor both localandglobalpublichealth sectors.With nearly one-thirdof isolates showing reduced sensitivityto keyantibiotics,the imperativeforinnovative surveillanceandpersonalizedtreatmentapproachescannotbe overstated.AsH.pyloricontinues topose significant risks related togastrointestinal disorders including peptic ulcersandgastric cancer,multisectoralcollaborationamongclinicians,researchers,andhealth authorities remains paramount.To safeguard future generations’access toeffective therapies,this study underscoresan urgent calltoactiontowardsresponsibleantibiotic stewardship,enriched diagnostics,andcomprehensiveinfectioncontrolmeasuresacrossChinaandbeyond.