Understanding Autoimmune Encephalitis: Novel Clinical Observations from Changsha
A pioneering investigation carried out at a prominent medical institution in Changsha, China, has provided valuable revelations regarding the clinical presentation and short-term prognosis of autoimmune encephalitis (AE), a multifaceted neurological disorder that remains challenging to diagnose and treat. With an increasing global incidence affecting diverse age groups, this focused single-center cohort study offers fresh insights into the varied symptom profiles and patient outcomes associated with AE. Published in the esteemed journal Frontiers, these findings not only deepen our comprehension of this debilitating illness but also highlight critical avenues for enhancing diagnostic accuracy and therapeutic approaches worldwide.
Diverse Clinical Features and Subtype-Specific Manifestations
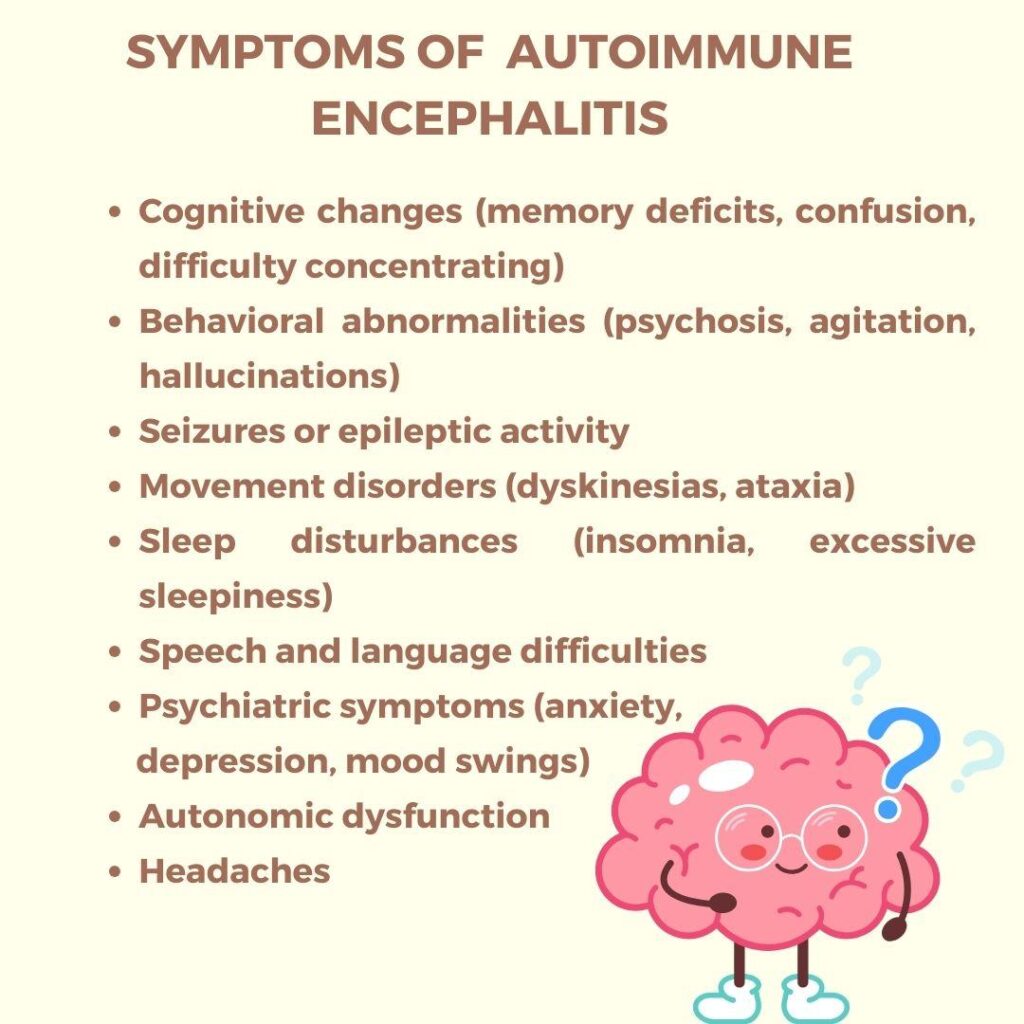
The Changsha cohort revealed a broad spectrum of symptoms reflecting the heterogeneous nature of autoimmune encephalitis. Key neurological and psychiatric manifestations identified include:
- Seizure activity: A predominant feature observed in many patients, often presenting as recurrent episodes.
- Cognitive disturbances: Impairments involving memory retention, attention span, and executive functions were frequently reported.
- Mental health challenges: Symptoms such as anxiety disorders, mood fluctuations, and psychotic episodes underscored the neuropsychiatric complexity inherent to AE.
- Motor impairments: Weakness coupled with coordination difficulties complicated rehabilitation efforts for affected individuals.
The study further delineated distinct clinical patterns among major AE subtypes. For instance, NMDA receptor antibody-mediated encephalitis typically manifested with acute psychiatric symptoms alongside seizures within days to weeks. Conversely, LGI1 antibody-associated encephalitis exhibited more insidious onset characterized by progressive memory deficits and sleep disturbances over several months. The table below encapsulates these subtype-specific differences:
| Subtype | Main Clinical Features | Typical Onset Timeline |
|---|---|---|
| NMDAR Encephalitis | Seizures; prominent psychiatric symptoms; autonomic dysfunctions | Soon after symptom emergence (days to weeks) |
| LGI1 Encephalitis | Cognitive decline; seizures; disrupted sleep patterns | Gradual progression (weeks to months) |
Key Prognostic Indicators Influencing Short-Term Recovery Outcomes
An extensive evaluation within this patient group identified several prognostic factors crucial for predicting short-term recovery trajectories in autoimmune encephalitis cases. Notably:
- Younger age at diagnosis (<40 years): Associated with significantly better recovery prospects compared to older patients.
- Disease severity upon initial presentation: Patients exhibiting milder neurological impairment tended toward more favorable outcomes. li >
- < strong > Early responsiveness to first-line immunotherapies : strong > Positive reactions particularly to corticosteroid treatment correlated strongly with improved prognosis . li >
- < strong > Duration before diagnosis : strong > Symptom persistence beyond four weeks prior to intervention was linked with poorer recovery rates . li >
- < strong > Presence of additional autoimmune conditions : strong > Comorbidities complicated disease course , reducing likelihood of full remission . li >
The following table summarizes how these factors relate quantitatively to patient outcomes :
< th > Prognostic Factor< / th >< th > Favorable Outcome (%)< / th >< th > Unfavorable Outcome (%)< / th > tr > thead >< tbody >< tr >< td ><40 years old< / td >< td >70%< / td >< td >30%< / td > tr >< tr >< td ><4 weeks symptom duration< / td >< td >75%< / td />< </tr></tbody></table> Advancing Diagnostic Precision and Therapeutic Approaches Based on Emerging Evidence from Changsha Study
The implications drawn from this comprehensive research emphasize refining current clinical protocols for diagnosing and managing autoimmune encephalitis effectively:
- Such initiatives foster international cooperation essentialfor tackling complex disorders like AE effectively.
Concluding Thoughts on Enhancing Autoimmune Encephalitis Care Worldwide
In conclusion,the detailed analysis conducted at this leading Chinese center enriches our understandingof autoimmune encephalitissymptomatologyandshort-term prognosis.By meticulously examiningpatient demographics,symptom duration,and treatment responses,the researchers have pinpointed critical determinants influencing disease trajectory.Early identification coupledwith individualized therapy emergesas paramountfor improving patient outcomes.As awareness grows globally aboutthis once underrecognized condition,new research inspiredby studies such as this will undoubtedly refine management paradigms,fostering hopefor enhanced qualityof lifeamong those affected.
Ongoing investigations into related neuroimmunological disorders continue expanding knowledge bases essentialfor future breakthroughs.
Ultimately,this evolving landscape calls for sustained education efforts aimedat clinicians,patients,and caregivers alike,to ensure timely recognition,treatment adherence,and comprehensive support systems remain integral components in combatingthe challenges posed by autoimmune encephalitis worldwide.