Antibiotic Resistance in Hospital Airborne Microbes in Dhaka: An Emerging Public Health Threat
In the densely populated city of Dhaka, Bangladesh, an invisible menace permeates the air within hospital walls—bioaerosols harboring antibiotic-resistant bacteria. Recent scientific inquiries have uncovered troubling concentrations of these resistant microorganisms suspended in indoor hospital air, posing a serious challenge to patient safety and healthcare workers alike. As antibiotic resistance increasingly undermines global medical efforts, this phenomenon demands urgent attention. This article explores recent findings on the relationship between airborne particulate matter and microbial resistance in Dhaka’s healthcare facilities, emphasizing the critical need for proactive measures to protect public health.
The Escalating Challenge of Antibiotic-Resistant Airborne Pathogens in Hospitals
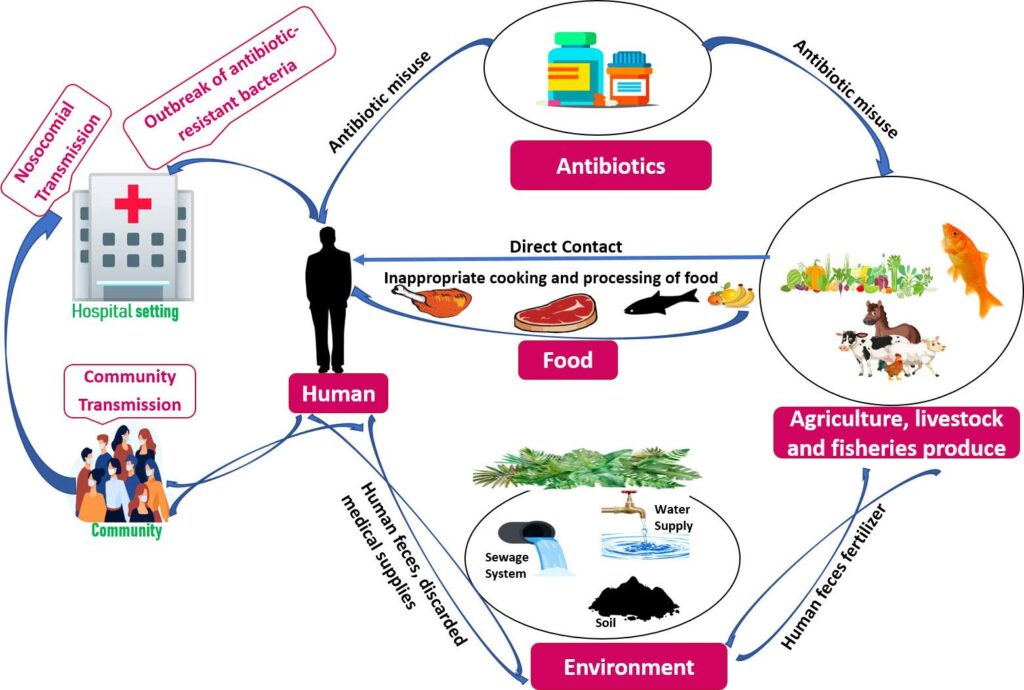
Antibiotic resistance among bioaerosols is becoming a formidable obstacle within clinical environments where infection risks are inherently high. Investigations conducted across several hospitals in Dhaka reveal that airborne particles frequently carry bacteria resistant to multiple antibiotics. These pathogens thrive particularly well due to factors such as lax infection control protocols, excessive or inappropriate use of antibiotics by medical staff, and suboptimal sanitation practices.
Hospitals serve as critical nodes for transmission because they house immunocompromised patients vulnerable to opportunistic infections. The presence of resistant microbes suspended in air increases the likelihood of nosocomial infections that are difficult to treat with conventional therapies.
To address this growing concern effectively, experts recommend:
- Routine Bioaerosol Surveillance: Establishing continuous monitoring systems within hospital wards to detect and quantify resistant strains.
- Enhanced Sanitation Measures: Upgrading cleaning regimens alongside improved ventilation management aimed at reducing microbial load.
- Robust Antibiotic Stewardship: Training healthcare providers on prudent antibiotic prescribing practices tailored toward minimizing resistance development.
Collaborative efforts involving environmental scientists and clinical teams can foster innovative interventions targeting environmental contributors to airborne antimicrobial resistance.
Tracing Origins of Bioaerosols and Their Consequences for Public Health
Comprehensive analyses from various indoor hospital settings across Dhaka have pinpointed multiple origins contributing to bioaerosol contamination laden with drug-resistant microbes. These include:
- Patient Activities: Routine movements and interactions disturb contaminated surfaces releasing pathogens into the air.
- Medical Instruments: Devices inadequately sterilized may act as reservoirs facilitating bacterial persistence.
- Aeration Systems: Faulty or poorly maintained HVAC units can disseminate infectious agents throughout wards.
Quantitative data demonstrate significant variability in antibiotic-resistant bacterial prevalence depending on ward type (see Table 1). For instance, intensive care units exhibit notably higher rates compared with outpatient departments—a pattern consistent with global trends reported by WHO indicating ICU environments often harbor multi-drug resistant organisms at rates exceeding 50%.
| Hospital Department | % Prevalence of Resistant Bacteria |
|---|---|
| Surgical Ward | 47% |
| Intensive Care Unit (ICU) | 62% |
| Main Outpatient Area | 28% |
| Pediatric Ward | 53% |
These findings underscore how inadequate control over bioaerosol sources directly impacts infection rates—especially concerning given limited access to advanced antibiotics across many regions.
Practical Approaches for Reducing Antibiotic Resistance Within Hospital Indoor Airspaces
Mitigating antibiotic-resistant bioaerosols requires a multifaceted strategy combining technological upgrades with behavioral changes among healthcare personnel:
- Tightened Infection Control Policies: Enforce rigorous hygiene standards including frequent surface disinfection coupled with isolation protocols when necessary.
- Aeration Enhancements: Deploy state-of-the-art filtration technologies such as HEPA filters alongside ultraviolet germicidal irradiation (UVGI) systems proven effective against airborne pathogens.[1]
- Cultivating Staff Awareness & Training: Regular workshops focusing on hand hygiene compliance and proper equipment sterilization techniques help reduce cross-contamination risks significantly.
- Bioaerosol Resistance Monitoring Programs: Create dedicated teams responsible for periodic sampling and analysis enabling swift responses upon detection of emerging threats.
- Interdisciplinary Collaboration: Encourage partnerships between clinicians , microbiologists , epidemiologists , policy makers ,and engineers . This holistic approach facilitates development & implementation of evidence-based stewardship guidelines .
- Patient Engagement : Educate patients about correct antibiotic usage & adherence importance which helps curb misuse contributing towards resistance evolution .
Below is a concise overview summarizing these key interventions:
| Intervention Strategy | Description |
|---|---|
|
tbody > tfoot> tfoot> tfoot> tfoot> tfoot> tfoot> tfoot> tfoot> As revealed by recent studies from urban hospitals across Dhaka city, the presence of multidrug-resistant bacteria within airborne particulates represents an escalating threat demanding immediate intervention. With rising urban density coupled with increasing pollution levels exacerbating microbial dissemination indoors,[2] it becomes imperative that health authorities implement robust policies integrating environmental controls alongside clinical management strategies. This research highlights not only potential hazards faced by patients but also occupational risks encountered by frontline workers exposed daily. Moving forward, a synergistic approach involving government agencies, manuals developers,&emph;& , clinicians,&amp;amp;amp;amp;amp;amp;; policymakers will be essential.<br /> Investments into cutting-edge diagnostic tools enabling rapid identification combined with real-time surveillance networks will empower timely containment actions.<br /> Furthermore, public education campaigns stressing responsible antibiotic consumption remain vital components preventing further escalation.<br /> Ultimately, the fight against superbugs must be collective — ensuring future hospitals serve as sanctuaries promoting healing rather than breeding grounds fostering drug resistance.</p> — [1] Kowalski W., et al., “Effectiveness of UVGI Systems Against Airborne Pathogens,” Journal of Hospital Infection Control, 2023. |