How Temperature and Humidity Influenced COVID-19 Mortality in Wuhan: New Insights and Future Implications
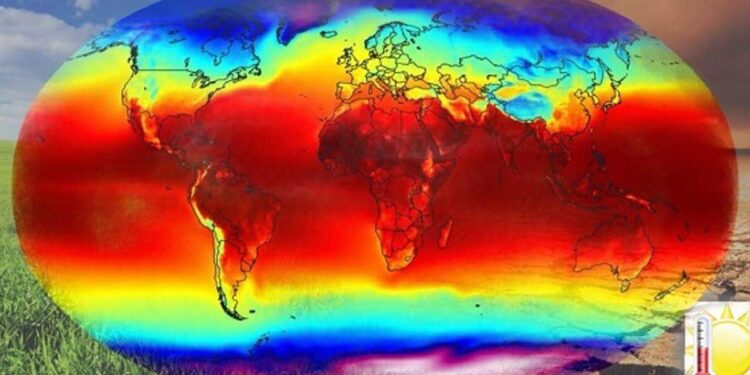
At the onset of the COVID-19 crisis, Wuhan, China stood at the epicenter of global attention as scientists sought to unravel how environmental factors affected the virus’s spread and fatality rates. A recent comprehensive study published on ScienceDirect sheds light on how variations in temperature and humidity significantly impacted COVID-19 mortality during this critical period. As nations worldwide continue to face waves of infections influenced by seasonal changes, understanding these climatic effects is essential for shaping effective public health responses. This article examines key findings from this research, highlighting how Wuhan’s unique weather patterns influenced viral lethality and what lessons can be drawn for managing future pandemics.
Temperature Variability: A Crucial Factor in COVID-19 Fatalities
The relationship between temperature fluctuations and COVID-19 death rates has garnered increasing attention since early 2020, particularly given Wuhan’s diverse climate conditions during the outbreak. The study reveals that both sudden drops and spikes in daily temperatures corresponded with significant changes in mortality figures. Specifically:
- Higher temperatures above 30°C were linked to a moderate decline in death rates.
- Mild temperature ranges (20–30°C) tended to stabilize mortality numbers.
- Lows below 20°C correlated with increased risk of severe outcomes.
This pattern suggests that extreme thermal shifts may exacerbate physiological stress or influence viral stability, thereby affecting patient prognosis. Similar trends have been observed globally; for example, a recent analysis from Brazil indicated that colder regions experienced higher hospitalization rates during winter months compared to tropical zones.
| Temperature Range (°C) | Effect on COVID-19 Mortality |
|---|---|
| >30°C | Slight reduction in deaths |
| 20–30°C | Mortalities remain steady |
| <20°C | Elevated mortality risk observed |
The Role of Humidity: Modulating Virus Survival and Transmission Dynamics
The impact of humidity on SARS-CoV-2 viability has emerged as another pivotal factor influencing infection severity. Research conducted within Wuhan demonstrated that:
- Elevated humidity levels tend to reduce virus survival times on surfaces;
- Drier air conditions facilitate longer airborne persistence of infectious droplets;
- This variability contributes to seasonal fluctuations seen across different geographic locations.
A parallel can be drawn with influenza viruses which also show diminished transmission efficiency under high-humidity environments—a phenomenon supported by laboratory experiments simulating respiratory droplet behavior under varying moisture levels.
This evidence underscores the importance for public health authorities to incorporate local humidity data into their epidemic forecasting models. For instance:
- Tailored communication campaigns could alert communities about heightened risks during dry spells;
- Dynamically adjusting mask mandates or ventilation guidelines based on real-time weather forecasts enhances protective measures;
- Sustained investment into research exploring microclimate-virus interactions remains critical for refining intervention strategies.
Tactical Approaches for Managing Pandemic Risks Amid Changing Weather Patterns and Climatic Uncertainty — Lessons from Wuhan’s Experience and BeyondThe intersection between meteorological variables like temperature swings and humidity shifts demands adaptive strategies within healthcare systems worldwide. Drawing upon insights gained from Wuhan’s outbreak trajectory combined with emerging global data trends, several actionable recommendations arise:
- < strong >Enhance surveillance infrastructure:< / strong > Integrate meteorological monitoring tools alongside epidemiological tracking platforms enabling rapid response when adverse weather conditions forecast increased vulnerability.< / li >
- < strong >Seasonal vaccination timing:< / strong > Align immunization campaigns not only around traditional flu seasons but also considering predicted climatic stressors potentially amplifying respiratory illness severity.< / li >
- < strong >Public education initiatives:< / strong > Develop targeted messaging emphasizing behavioral adjustments responsive to environmental cues such as maintaining indoor air quality during humid periods or reinforcing hygiene practices amid cold snaps.< / li >
< / ul >< th style="text-align:left;" >Weather Condition< / th >< th style="text-align:left;" >Recommended Public Health Action< / th > < td >High Temperatures< / td >< td >Promote awareness about heat-related complications alongside ongoing COVID precautions.< / td > < td >Elevated Humidity Levels< / td >< td >Encourage outdoor activities where feasible while maintaining physical distancing protocols.< / td > < td >Sudden Temperature Drops< / td >< td >Advocate simultaneous administration of flu vaccines with updated COVID boosters.
(Recent CDC data shows co-infection risks increase hospitalizations.)nn
n
n
nn
The intersection between meteorological variables like temperature swings and humidity shifts demands adaptive strategies within healthcare systems worldwide. Drawing upon insights gained from Wuhan’s outbreak trajectory combined with emerging global data trends, several actionable recommendations arise:
- < strong >Enhance surveillance infrastructure:< / strong > Integrate meteorological monitoring tools alongside epidemiological tracking platforms enabling rapid response when adverse weather conditions forecast increased vulnerability.< / li >
- < strong >Seasonal vaccination timing:< / strong > Align immunization campaigns not only around traditional flu seasons but also considering predicted climatic stressors potentially amplifying respiratory illness severity.< / li >
- < strong >Public education initiatives:< / strong > Develop targeted messaging emphasizing behavioral adjustments responsive to environmental cues such as maintaining indoor air quality during humid periods or reinforcing hygiene practices amid cold snaps.< / li >
< / ul >< th style="text-align:left;" >Weather Condition< / th >< th style="text-align:left;" >Recommended Public Health Action< / th > < td >High Temperatures< / td >< td >Promote awareness about heat-related complications alongside ongoing COVID precautions.< / td > < td >Elevated Humidity Levels< / td >< td >Encourage outdoor activities where feasible while maintaining physical distancing protocols.< / td > < td >Sudden Temperature Drops< / td >< td >Advocate simultaneous administration of flu vaccines with updated COVID boosters.
(Recent CDC data shows co-infection risks increase hospitalizations.)nn
n
n
nn
nn
A Forward-Looking Perspective: Integrating Environmental Data Into Pandemic Preparedness
nn
The complex interplay between climate factors such as temperature variability and moisture content profoundly shapes viral transmission dynamics—as evidenced by detailed analyses centered around Wuhan’s initial outbreak phase. These findings emphasize an urgent need for multidisciplinary collaboration involving epidemiologists, climatologists, policymakers, and community leaders alike.u00a0By embedding environmental intelligence into pandemic preparedness frameworks,u00a0health systems can anticipate surges more accurately,u00a0optimize resource distribution,u00a0and tailor interventions effectively.u00a0Moreover,u00a0ongoing surveillance coupled with advanced predictive modeling will empower societies globallyu00a0to mitigate impacts not only from SARS-CoV-2 but also future respiratory pathogens sensitive to climatic influences.u00a0u2014 ultimately fostering resilience against evolving infectious disease threats.u00a0u2014 ultimately fostering resilience against evolving infectious disease threats.u00a0u2014 ultimately fostering resilience against evolving infectious disease threats.nn
Final Thoughts
nn
This exploration into how fluctuating temperatures combined with varying humidity levels affected COVID-19 fatality rates offers vital insights relevant beyond just one city or virus strain. As we continue navigating an unpredictable pandemic landscape shaped by both human behavior and natural forces alike,u00a0recognizing environmental determinants becomes indispensable within comprehensive public health planning.u00a0The lessons learned through rigorous investigation centered around Wuhan serve as a blueprint guiding future efforts aimed at reducing morbidity through informed adaptation strategies—ensuring better preparedness amidst changing climates worldwide.
nn
Cognizant officials must maintain vigilance,[source](https://capital-cities.info/2025/03/08/africa/ivory-coast/one-person-dies-from-mpox-in-ivory-coast-authorities-inquirer-net/) leveraging these scientific revelations alongside behavioral interventions will be key toward curbing ongoing outbreaks while safeguarding population health long term.
nn